EVEN IN HEALTHY KIDNEYS, URATE REMOVAL IS COMPLEX
Here’s a look inside the predominant and imperfect role the kidneys play in processing uric acid.
Metabolism and the uricase enzyme
- A weak organic acid, uric acid is the final product of human purine metabolism1
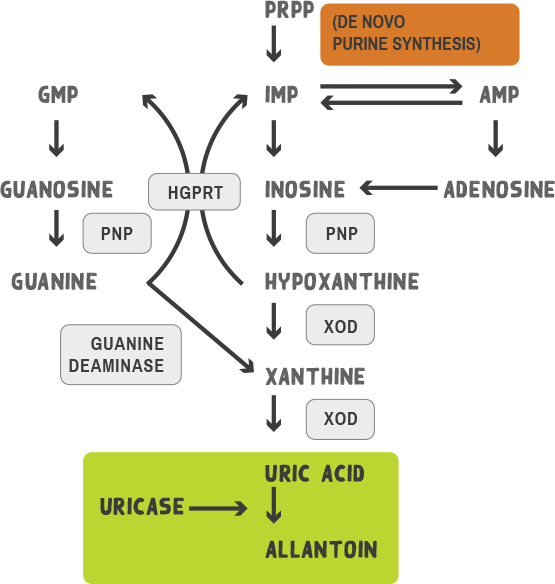
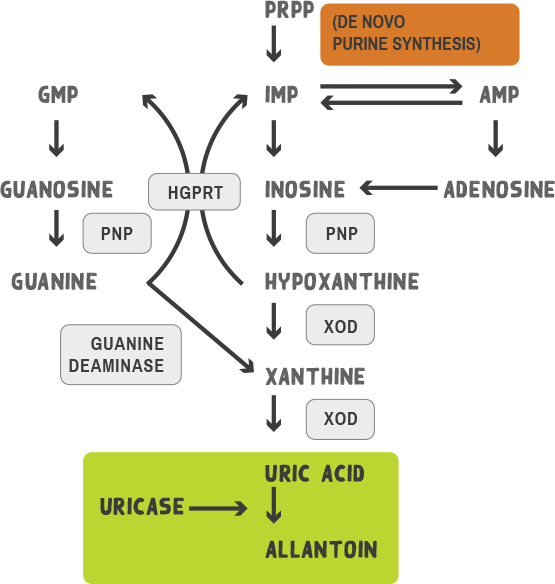
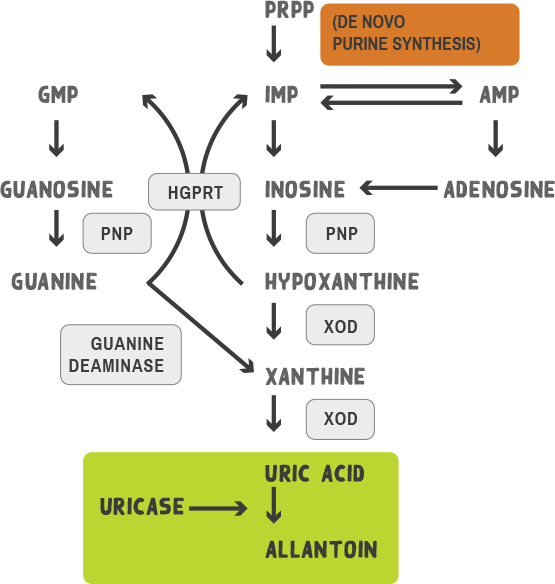
AMP, adenosine monophosphate; GMP, guanosine monophosphate; HGPRT, hypoxanthine‑guanine phosphoribosyltransferase; IMP, inosine monophosphate; PNP, purine nucleoside phosphorylase; PRPP, 5‑phosphoribosyl 1‑pyrophosphate; XOD, xanthine oxidase.
Graphic adapted from Terkeltaub R, et al.Arthritis Res Ther. 2006;8(suppl 1):S4.
- A weak organic acid, uric acid is the final product of human purine metabolism1
- During evolution, humans lost the enzyme uricase that converts uric acid into allantoin and must rely on the kidneys for daily uric acid excretion2
- Allantoin is a water‑soluble metabolite that is up to 10x more readily excreted through the urine than uric acid3
Graphic adapted from Terkeltaub R, et al. Arthritis Res Ther. 2006;8(suppl 1):S4.
Elimination Roles
- The kidneys eliminate two-thirds of uric acid from the body. The gastrointestinal tract eliminates the remaining one‑third4
- Net renal excretion of urate appears to be dependent on the balance between filtration, secretion, and reabsorption5
- Almost all uric acid is filtered at the glomerulus. Reabsorption and secretion occur within the proximal tubule5
- Despite nearly complete filtration of urate at the glomerulus, uric acid clearance averages only 8–12% that of inulin or creatinine, reflecting the net reabsorption of about 90% of filtered urate1
Graphic adapted from Choi HK, et al. Ann Intern Med. 2005;143:499-516.
Graphic adapted from Choi HK, et al. Ann Intern Med. 2005;143:499-516.
Roles of urate transporters
Filtered urate is greatly reabsorbed in the proximal tubules in humans. The reabsorption and secretion processes depend on specific transporter molecules that reside in these membranes.6
Graphic adapted from Hyndman D, et al. Curr Rheumatol Rep. 2016;18(36):34 and Reginato AM, et al. Nat Rev Rheumatol. 2012;8(10):610-621.
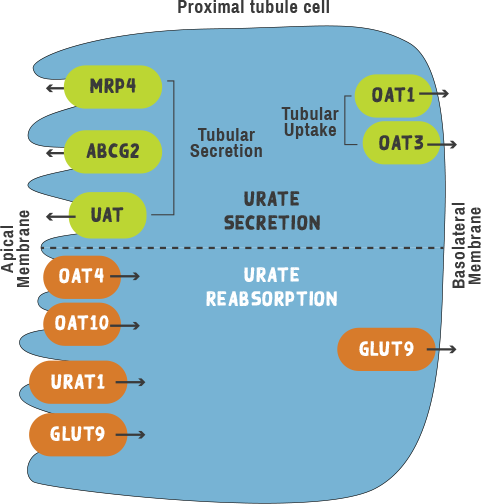
Graphic adapted from Hyndman D, et al. Curr Rheumatol Rep. 2016;18(36):34 and Reginato AM, et al. Nat Rev Rheumatol. 2012;8(10):610-621.
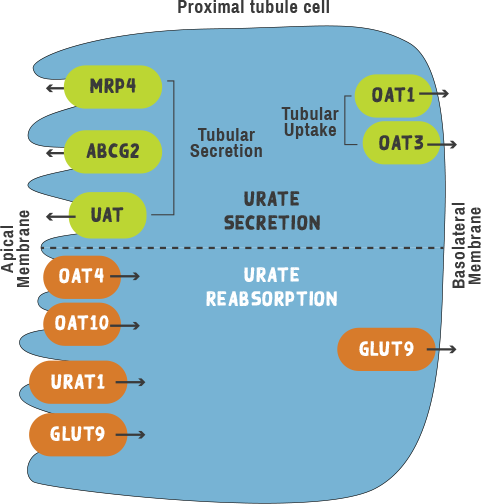
URATE REABSORPTION TRANSPORTERS
OAT4 (organic anion transporter)
- Capable of transporting organic anions, including hormones and various drugs, OAT4 transports urate on the apical membrane of the proximal tubule7
OAT10 (organic anion transporter)
- Present on the apical side of the kidney proximal tubule, OAT10 transports urate with low affinity7
- Similar to URAT1, transport of urate is stimulated by exchange of lactate, pyrazinoate, and nicotinate7
URAT1 (human urate anion transporter)
- Play an important role in both hyperuricemia and gout7
- Persons deficient in functional URAT1 have extremely low serum urate levels7
- Responsible for urate reabsorption from the apical (luminal) side of the proximal tubule7
GLUT9 (glucose transporter)
- Strongly linked to hyperuricemia and gout7
- Responsible for the flow of reabsorbed urate out from the interior of the proximal tubule cells back to the blood7
- GLUT9 has been reported to be a fructose transporter and potentially a fructose‑urate exchanger8 and was reported to function as an efflux transporter of urate from tubular cells and to affect serum urate concentration9
SECRETION TRANSPORTERS
MRP4 (multidrug resistance protein)
- Proposed to mediate secretion of urate and other organic anions across the apical membrane of human renal proximal tubular cells6
- Serves as an ATP‑dependent unidirectional efflux pump for urate with multiple allosteric substrate binding sites6
ABCG2 (ATP‑binding cassette super‑family G member 2)
- Expressed in the membrane of proximal tubules of the kidney, functional studies suggest that ABCG2 has a role in the excretion of uric acid levels as a urate transporter8
UAT (urate transporter)
- Believed to be a multimeric protein, UAT is expressed ubiquitously and localizes to the apical side of the proximal tubule in the kidney6
- As it is related to various functions that appear to be unrelated to urate transport, further studies are needed to determine the precise role of UAT in urate metabolism6
OAT1 and OAT3 (organic anion transporters)
- Function as anion‑dicarboxylate exchangers at the basolateral membrane of the proximal tubule10
- Both have been shown to transport urate, and it is likely that they contribute to basolateral urate uptake rather than efflux6
What happens to urate clearance when renal function declines?
REFERENCES
-
Terkeltaub R, et al. Arthritis Res Ther. 2006;8(suppl 1):S4.
-
Eleftheriadis T, et al. J Adv Res. 2017;8:555-560.
-
McDonagh EM, et al. Pharmacogenet Genomics. 2014;24:464-476.
-
Maiuolo J, et al. Int J Cardiol. 2016;213:8-14.
-
Eraly SA, et al. Physiol Genomics. 2008;33:180-192.
-
Hediger MA, et al. Physiology. 2005;20:125-133.
-
Hyndman D, et al. Curr Rheumatol Rep. 2016;18:34.
-
Reginato AM, et al. Nat Rev Rheumatol. 2012;8:610-621.
-
Richette P, et al. Lancet. 2010;375:318-328.
-
Choi HK, et al. Ann Intern Med. 2005;143:499-516.
